8. Severe hypoglycaemia
Severe hypoglycaemia does not generally occur frequently in children with diabetes where children are monitored and supervised. However changes to usual routines, usual activity levels or usual insulin requirements can increase the risk of severe hypoglycaemia.
What causes severe hypoglycaemia?
Severe hypoglycaemia most often occurs when there is a combination of the following:
Not eating enough carbohydrate (food refusal or during periods of illness)
Delayed or missed meals
Too much insulin
More exercise or activity than usual
Alcohol - see transition resources for young people
If an episode of mild - moderate hypoglycaemia is not treated in a timely manner, the blood glucose levels can continue to fall to a level where a child becomes unconscious or passes out. Sometimes when this happens there is twitching of the arms and legs which may look like a convulsion/fit.
If there is a prolonged period (for example over a week or so) when the blood glucose levels are frequently under 4 this can increase the risk of severe hypos. This may be during periods when regular routines are disrupted; such as holidays (especially swimming and hot pools), birthday parties (especially pool parties), overseas travel with time changes, starting a new sport without adjusting insulin or food or during periods of illness. These are times when it is essential to undertake more frequent blood glucose testing. Your diabetes team can offer support and advice in establishing an individualised plan for any changes in the usual daily routine.
Symptoms
Extremely drowsy or confused
Unconscious or passed out
Having a fit or convulsion
What to do if your child is unconscious
It is important to place your child in the "recovery position" on their side. This will protect their airway and allow them to breathe normally. Move away anything dangerous (for example large furniture, heaters etc.)
It is important that you check the blood glucose level as quickly as possible. If the level is under 4 then you need to assume that your child is having a severe hypoglycaemic episode. If you are unable to test then treat as a severe low.
If the level is above 4, your child may be unconscious for a reason not related to diabetes (for example, they may have fallen and had a head injury).
In either case, once you have checked the blood glucose level, call an ambulance stating that your child is unconscious and has Type 1 diabetes. They will want to know what the blood glucose level is. It is unlikely your child will need to go to hospital but the ambulance staff will be able to support you with treatment and care of your child.
Do not put anything in your child's mouth such as food, drink or glucose gel.
Glucagon Injection
Glucagon is a hormone that increases the level of glucose in the blood. It allows stored sugar from the liver (glycogen) to be converted to glucose and then released into the blood stream.
Treatment for severe hypoglycaemia using the Glucagon Kit
You can read a transcript of this video here.
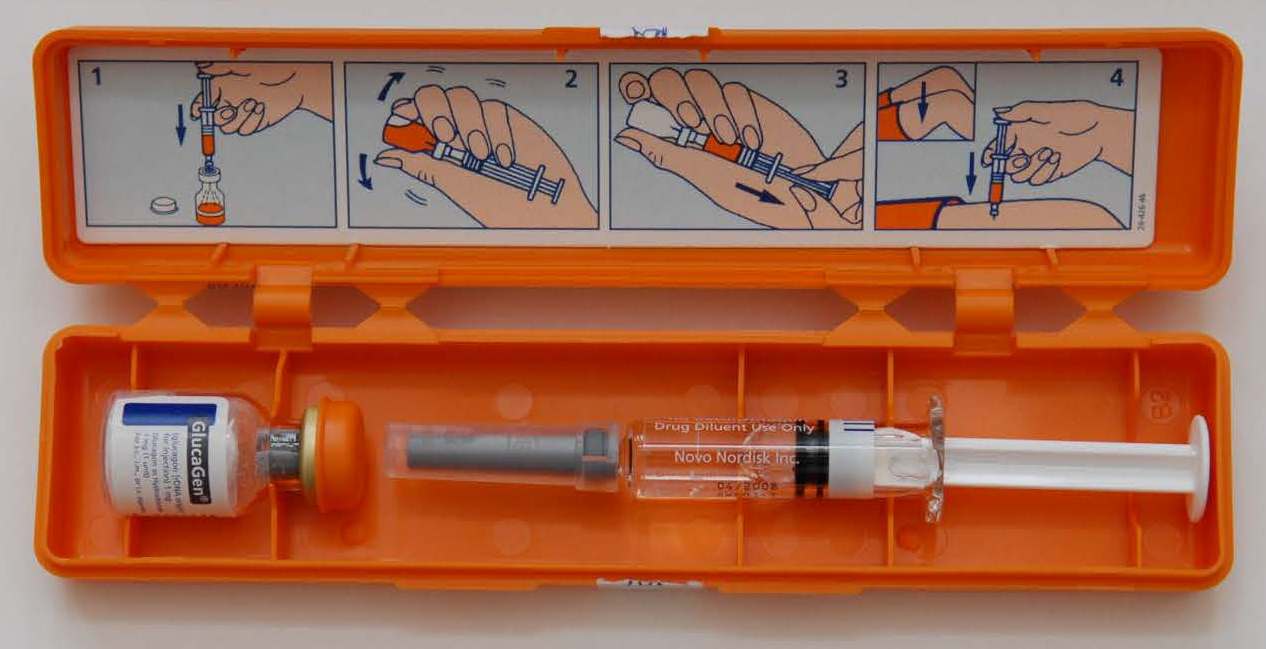
Instructions are in picture form on the inside of the lid. Inside the orange box you will find a syringe filled with sterile water and a glass vial/bottle containing glucagon powder.
Take the orange cap off the glass vial and the grey cap off the top of the syringe and carefully inject all of the sterile water into the vial.
Without taking the needle out, gently swirl the solution then turn the vial and the syringe upside down.
Holding the vial in one hand, use your other hand to pull down on the white plunger so that the mixture comes back into the syringe. If your child is under 5 years or less than 25kgs give 0.5ml. If your child is older than 5 years or more than 25kgs give all of it.
Inject at a 90 degrees angle into the large thigh muscle at the side of the upper leg
After giving Glucagon
You will not harm your child by giving glucagon. Your child is unconscious and will not feel the the injection. The most important thing to focus on is getting the blood glucose levels into a safe range.
The glucagon takes 5-10 minutes to start working by which time your child will begin to wake up.
Check the blood glucose level once your child is awake.
Once your child is able to swallow follow usual hypoglycaemia treatment guidelines.
Give fast acting carbohydrate such as a juice drink (15-20 grams) and re-check the level 10-15 minutes later.
Repeat this until the blood glucose level is above 5 mmol
Once the blood glucose level is above 5 mmol/l give your child some long-acting carbohydrates such as dry toast or crackers.
Your child may feel sick or vomit. If your child is vomiting, keep offering sips of sweet fluids (juice, lemonade, cordial) until food can be tolerated. Keep checking the blood glucose levels every 15minutes if your child is vomiting or refusing to eat.
Once your child is fully recovered call the diabetes doctors on 09631 0790 option 1. The daily doses of insulin will need to be reduced and it is important that daily contact is maintained via telephone for the period immediately following a severe hypo. The diabetes team may request to see your child in clinic earlier than planned.
You will need to obtain a prescription for a replacement glucagon kit either via your GP or the diabetes team.
In most cases of severe hypoglycaemia admission to hospital is not required if there has been a good response to the glucagon injection.
Prevention of Severe Hypoglycaemia
Regular blood glucose testing and close supervision is the best way to reduce the risk of severe hypoglycaemia.
When changes to routines occur, such as holidays, camps and day trips, try to plan the days in advance so meals and insulin are given close to usual times
Talk to your diabetes team about the possible need to decrease insulin doses if activity levels are going to be higher or different than usual.
When planning air travel of any kind, please talk to your diabetes team. Doses and timing of insulin doses may need to change if there are time zone changes and there are many ways to do this safely with guidance from your diabetes team.
If your child is over 5 years old and regularly doesn't feel any symptoms of hypoglycaemia when the blood glucose levels are under 4, contact your diabetes team to discuss further.
Let's go over the main points. Read this factsheet to make sure you understand the causes and treatment of severe hypoglycaemia. Read more...
Think you've got it sorted now?
If you and your parent/carer have read through the information above and watched the video, and you feel confident that you understand this topic, print off and fill in the evaluation form below (you might need to ask someone to print this off for you) and return to the nurse on your ward. If you have any questions, note them down on this form and your diabetes nurse specialist will discuss them with you.
Severe Hypoglycaemia: Evaluation
After reading this teaching module and watching the video, I:
| Yes | No | |
| Know the signs of a severe hypo | ||
| Know the reasons why a severe hypo might occur | ||
| Know how to place my child in the recovery position if unconscious | ||
| Understand that I need to do a blood glucose test if my child is unconscious before I call an ambulance | ||
| Know how to draw up the Glucagon injection | ||
| Know how much Glucagon to give and understand where and how to give it | ||
| Know how to care for my child after a severe hypo | ||
| Understand that it is important to talk to the diabetes team if my child has had a severe hypo | ||
| Understand that it is important to talk to the diabetes team if my child is starting a new sport, going to be more active, is not eating well or is unwell. |
Comments:
Date:
Name:
