7. Understanding Hypoglycaemia (Low Blood Sugar)
What is a Hypo?
Hypoglycaemia (often called a hypo) is when the blood glucose (sugar) level drops below 4 mmol/L.
What causes low blood sugar?
A hypo can happen when your tamaiti:
Doesn't eat enough carbohydrate
Misses or delays a meal
Has too much insulin
Does more activity or sport than usual
Drinks alcohol (applies to older rangatahi) - see transition resources for young people
Signs to watch for:
Signs of a hypo can look different for every tamaiti, but common ones include:
Looking pale
Headache
Shaky or weak
Sweaty
Dizzy or sleepy
Trouble concentrating
Changes in mood or behaviour
Crying, irritability, or tantrums (especially in younger tamariki)
Hunger
Confusion or blurred vision
Slurred speech
If you notice any of these signs, or if your tamaiti just isn't acting like themselves, check their glucose levels.
If the CGM number doesn't match how your tamaiti is behaving - or if hypos are happening often or not improving - do a fingerprick test to confirm.
You can read a transcript of this video here.
How to treat low blood sugar
Always carry fast-acting carbohydrate foods or drinks in case of a hypo. Your tamaiti should never be left alone during a hypo.
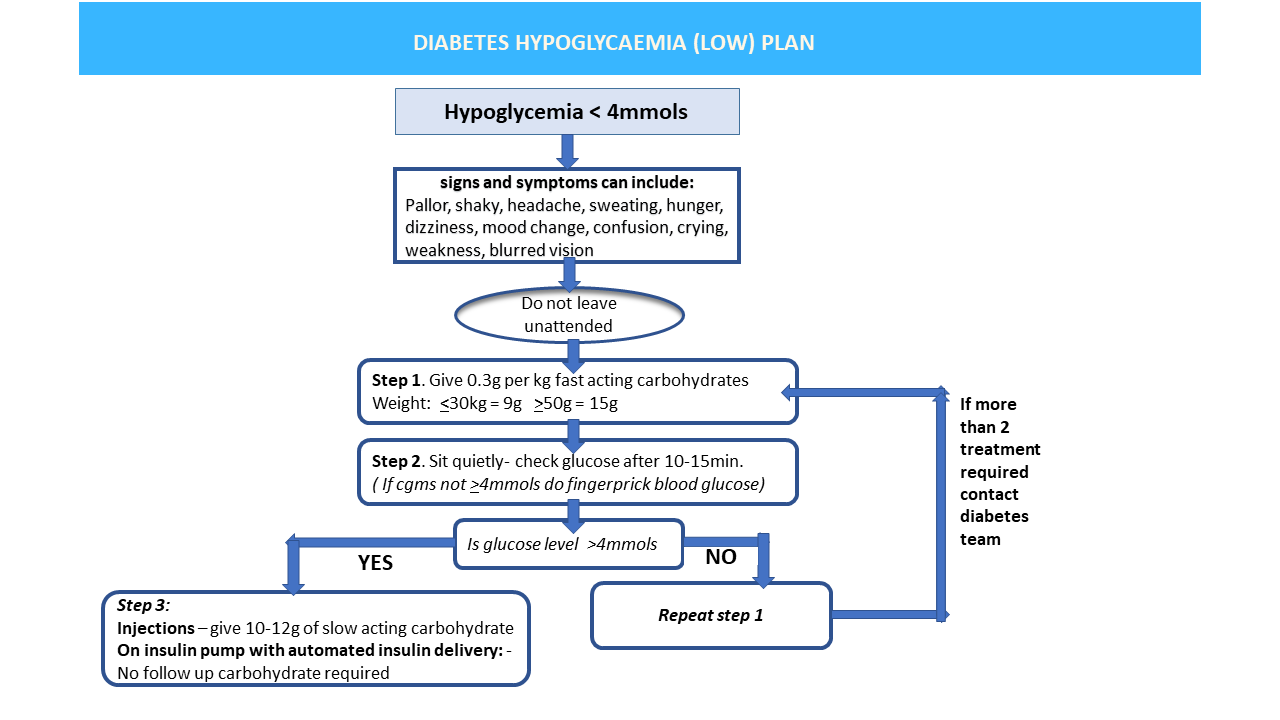
Step one: Give fast-acting carbohydrate
If blood glucose is under 4 mmol/L, give a fast-acting carbohydrate - about 0.3 grams per kilogram of your child’s body weight.
(To work this out: multiply your tamaiti’s weight by 0.3)
Some good options:
Pre-packed juice drinks
Dextrose or glucose tablets
Mentos
Honey
Regular (full sugar) fizzy drink
❗ Do not use chocolate to treat a hypo - it contains fat which slows down sugar absorption.
Step two: Rest, re-check, and fingerprick if needed
After giving the fast-acting carbohydrate:
Have your tamaiti sit quietly for 10-15 minutes.
Recheck their glucose level: If the reading is under 4 mmol/L, do a fingerprick to double-check. If the level is still low, repeat the fast-acting carbohydrate treatment.
Rest again for another 10–15 minutes, then check the level once more.
❗ If your tamaiti still has a reading below 4 mmol/L after two rounds of treatment, call your diabetes doctor or nurse for advice.
Step three: Follow-up snack (not required if on insulin pump)
Once the blood sugar is back above 4 mmol/L, your tamaiti might need a longer-acting carbohydrate snack (10–12 g), such as:
A piece of fruit
1-2 large crackers or 6 small crackers
A plain muesli bar or fruit bar
If it’s nearly mealtime, the meal itself will count as this snack.
Children on Insulin Pumps (using automated insulin delivery)
If your tamaiti is using an insulin pump, they do not usually need a follow-up snack unless told otherwise by your diabetes team.
That’s because the pump reduces insulin automatically when levels are low, helping glucose rise safely without overcorrecting.
If you’re unsure what’s best, ask your diabetes nurse or doctor for personalised advice.
Preventing night-time hypos
Hypos can happen overnight, especially if your tamaiti has:
Been more active or done extra sport
Eaten less than usual during the day
Been unwell
Tips to prevent night-time lows:
You might need to reduce insulin doses in the evening after big activity days – talk to your diabetes nurse or doctor
Alcohol increases the chance of overnight hypos (for rangatahi)
During the honeymoon phase (soon after diagnosis), some tamariki may have lower overnight readings (3.5–4 mmol/L) without it being a true hypo - check with your team if unsure
Hypoglycaemia unawareness - when they don't feel it
Some tamariki may have a low blood sugar but don’t notice any symptoms. This is called hypo unawareness.
Little ones may not yet know how to describe a hypo – so mātua and caregivers need to stay alert.
After a hypo, talk with your tamaiti about how it felt, to help them learn to recognise symptoms next time.
Older tamariki may develop hypo unawareness after frequent or unnoticed lows. Their body gets used to it, which can be dangerous.
❗ CGMS can detect lows before they get low enough to feel the symptoms however if your tamaiti is having blood sugars under 4 mmol/L frequently but isn’t noticing them, please discuss with your diabetes team.
Other important info
Your tamaiti should always wear a medical alert bracelet or ID that says they have diabetes.
Make sure whānau, teachers, and caregivers know what to do in case of a hypo.
Hypoglycaemia - an overview. Let's go over the main points we've just covered. Ready?
Think you've got it sorted now?
If you and your parent/carer have read through the information above and watched the videos, and you feel confident that you understand this topic, print off and fill in the evaluation form below (you might need to ask someone to print this off for you) and return to the nurse on your ward. If you have any questions, note them down on this form and your diabetes nurse specialist will discuss them with you.
Hypoglycaemia: Evaluation
After reading this teaching module and watching the videos, I feel confident in:
| Yes | No | n/a | |
| Understanding what causes a hypo | |||
| Recognising the possible signs/symptoms of a hypo | |||
| Understanding how to treat a hypo | |||
| Recognising when I should call the medical team for advice when treating a hypo | |||
| Knowing how to prevent a severe hypo |
Comments:
Date:
Name:
