Consult Liaison
About the Consult Liaison team
Kia ora and ngā mihi for your interest in Consult Liaison.
The Starship Consult Liaison team was established by Dr Louise Webster, Paediatrician and Child Psychiatrist, and Linda Chard, Clinical Psychologist in 1990 (in response to increasing concern from paediatricians and other staff regarding children’s emotional well-being while undergoing medical treatment). At the time these two clinicians provided a psychological/psychiatric assessment and treatment service to the whole of the Princess Mary Hospital and its outpatients – a busy job! From these beginnings our team has grown in size and scope: we now have more than 30 staff, most of whom are part-time and we see around 900 Starship tamariki, rangatahi and whānau each year.
We are based on Level 3 of the Starship where we have some dedicated therapy rooms and an administrative office.
Our services include mental health assessment and management of tamariki and rangatahi, including neuropsychological assessment for those who have had medical treatments which affect thinking and behaviour.
We provide a range of therapies including Family, Cognitive Behaviour, Child Psychotherapy, ACT, EMDR, medications and Supportive therapy. We can see parents for mental health assessments and will liaise with other services to help them get support. Where parents are not able to move off site we can provide a limited range of therapies to them as well.
Our staff includes Child & Adolescent Psychiatrists (three are also Paediatricians), Clinical Psychologists and Neuropsychologists, Child and Adult Psychotherapists and Nurse Specialists. Some staff have been funded by new initiatives in transplant and other areas.
We have a rotating duty system in which all staff take a turn on responding to inpatient referrals. All referrals are discussed in Multi-Disciplinary meetings where senior staff are present.
Why Consult Liaison?
Around 11% of New Zealand children have a chronic health condition: it is known that such conditions increase the rate of mental health disorder from 2.5 times baseline to more than 10 times, depending on the type of illness and the physical system affected
Modern medical technologies are providing remarkable improvements in the survival and life expectancy for those with previously fatal illnesses and trauma. These have resulted in new and often complex invasive treatment regimens which have high emotional, practical and ethical demands for children and whānau. Examples include transplants: bone marrow, cardiac, renal and liver as well as some intensive treatments for cancer and neurological disorders
In addition, multidisciplinary management of tamariki and rangatahi is now the norm: this means there is a focus on the whole child, rather than their medical management alone, and greater recognition and acceptance of psychological treatments and support
Who we see: our referral criteria
(Note some specialty teams have their own referral pathways)
1. Meets criteria for entry: complete referral
| Assessment and treatment of tamariki and rangitahi under the ongoing care of a Starship service who present with the following: |
|---|
| Significant child behavioural or emotional disorder or mental health disorder that impacts treatment for a health condition |
| Mental health safety issues: harm to self or others (Inpatients only, including Children’s ED). Outpatients refer to local Child & Adolescent mental health service especially if there are acute safety concerns. Assessment typically occurs once patients are medically stable unless there are immediate mental health safety concerns |
| Assessment and treatment of medically unexplained, complex or somatoform disorders |
| Rangatahi with Eating Disorders who have required admission due to medical instability or medical complications |
| Significant parent or whānau distress or coping difficulties in relation to the child’s illness and or treatment, beyond usual expected levels for a new or difficult diagnosis |
| Elective assessments for conditions or procedures that are associated with high mental health challenges such as transplant (Some teams have their own processes for pre-transplant assessment) |
| Consultation with ADHB Starship staff on complex cases where there are concerns for mental health/safety and/or psychiatric/psychological diagnostic queries, including child protection cases |
| Consultation for medical mediation |
2. More information required/other services may be more appropriate
| Acute procedural anxiety: Involve Hospital Play Specialists as first intervention, refer if this isn’t enough or if the situation is especially complex |
| Social issues/care and protection issues impacting on care: Social work assessment and Te Pururuahau with CLT involvement as needed |
| Current mental health or disability services are already in place: consult with family and team member/key worker before referral to CLT to avoid inconsistency or double-up of care. Examples include: Mental Health Services, Child & Adolescent Mental health services, Maternal Mental Health, Community Mental Health Centre, Disability services (CDS, EXPLORE), NGOs (e.g. Youth Horizon’s Trust, CANTEEN) |
| Complex and Persistent Pain: consult with the Starship pain team involvement for persistent pain; see Starship guidelines before referral |
| For medically unexplained, complex or somatoform disorders please consider completion of investigations and gain consent before referral. If an admission is pre-planned, please consult beforehand so we can ensure availability of staff |
3. Does not meet criteria for entry
| Outpatient tamariki/rangatahi without ongoing Starship involvement - please refer to local DHB Child & Adolescent Mental Health service |
| Siblings and extended whānau needing support: refer to NGO such as Parent to Parent/Starlight/Child Cancer Foundation |
| Consent has not been obtained (except for acute mental health emergencies where there are immediate concerns of harm to self or others) |
How to refer
Use the electronic referral system, making sure to specify Outpatient or Inpatient (Search for "consult").
We welcome discussion of referrals especially if these are complex or urgent and we can be contacted on 021-492403 between 8:30am and 4:30pm weekdays (Extension 23303 for administrative queries)
Outside of these hours cover is provided by the on-call psychiatry registrar backed by a child psychiatrist: call via the switchboard (phone 307 4949)
What’s our timeframe?
If urgent or complex, please call 021-492403 to discuss further
Inpatients
We aim to see patients where there are urgent safety concerns for self-harm or harm to others (patient or boarder parent) within 2 hours (Note that the team cannot guarantee an immediate crisis response and if necessary Code Orange should be used as per Starship and ADHB guidelines)
| Within 8 hours |
|---|
| Post-self-harm in medically stable patient requiring psychiatric assessment |
| Within 24 hours |
|---|
| Psychological or behavioural issues associated with high levels of distress or with compromise of medical management |
| Within 48 hours |
|---|
| Psychological or behavioural issues that present a diagnostic difficulty |
| Other referral issues |
Outpatient referrals
Are usually seen within 3-8 weeks
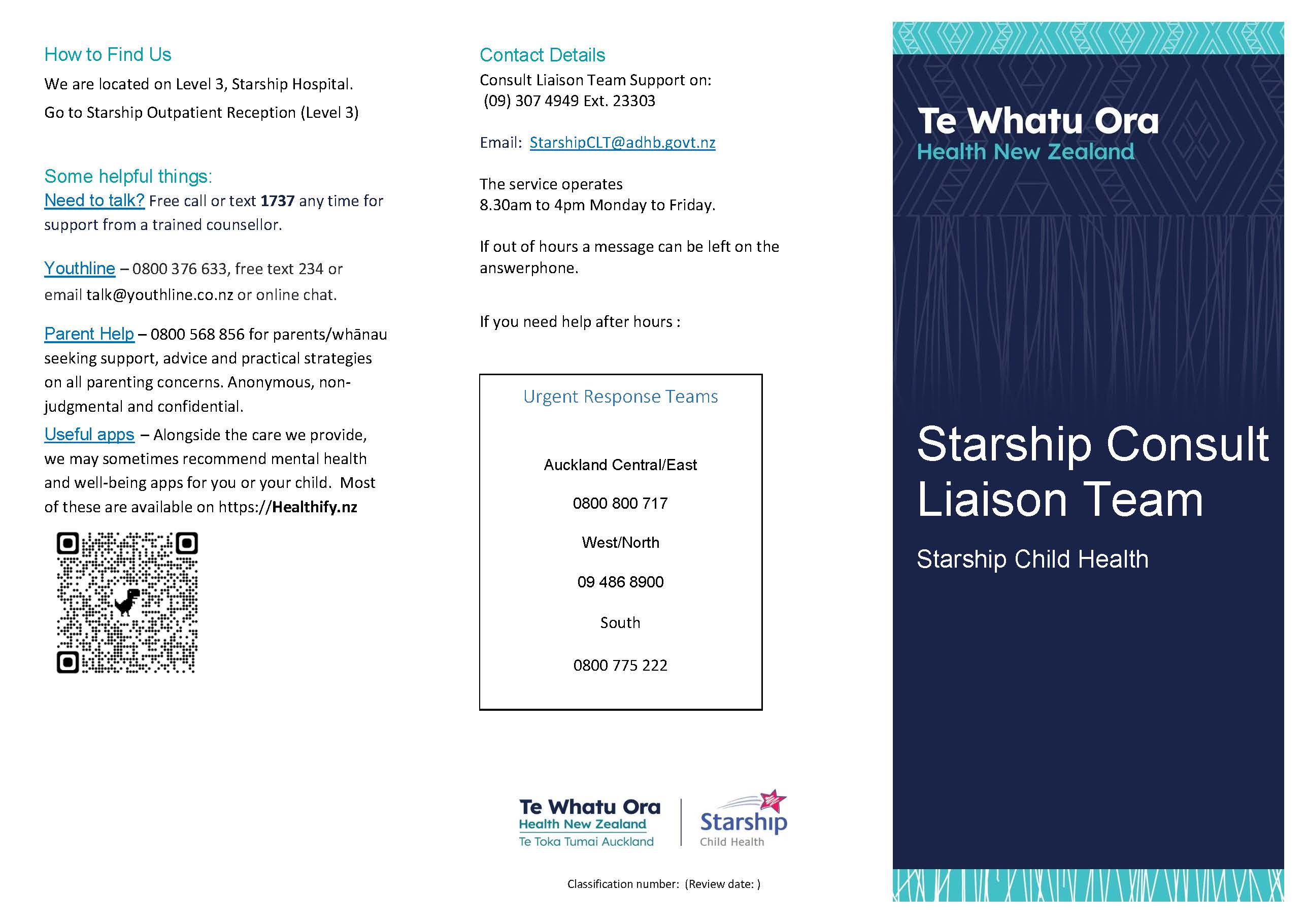
Click on the image below for a downloadable pdf brochure