Glucose monitoring systems
The New Zealand Context
Over the last few years there has been a rapid uptake and interest in glucose monitoring systems in New Zealand. Many people are using them or have questions about them. The Paediatric Society of New Zealand Clinical Network for Children and Young People’s Diabetes Services recognise this need and have put together this resource to explain how glucose monitoring systems work, the advantages and disadvantages, as well as providing a comparison of the systems available in New Zealand as at May 2019.
A Continuous Glucose Monitor (CGM) and a Flash Glucose Monitor (FGM) are medical devices for measuring glucose levels. They are used most often by individuals who have type 1 diabetes. CGM and FGM in children and youth may be useful if your child is not able to communicate or recognise symptoms of hypoglycaemia. They perform a similar function as a “finger prick” blood glucose meter (that is, it gives you information about glucose levels). A sensor is placed just under the skin surface and measures the glucose in the interstitial fluid – the fluid surrounding the cells.
There are, however, a few important differences between Continuous or Flash Glucose Monitoring Systems and finger prick checks:
Finger prick checks involve piercing the skin (e.g., the finger or toe) each time you check a blood glucose
CGM/FGM involves inserting a sensor under the skin which stays in place for several days
Finger prick readings measure glucose in a drop of blood
CGM/FGM measures glucose in the interstitial fluid just underneath the skin, the fluid that surrounds the cells (this result may lag 2 – 20 minutes behind blood glucose levels)
Finger prick glucose monitoring is like a snapshot; it captures a moment in time
CGM/FGM is like a movie; gives you a series of readings in real-time, as it repeatedly measures and reports glucose levels (the equivalent of performing 288 finger pricks each day). This gives you information about what’s happening between finger prick checks.
In short, finger prick blood glucose checking provides you with a glucose level for a single point in time. CGM/FGM is a useful tool to track glucose levels, which direction it’s going and how fast.
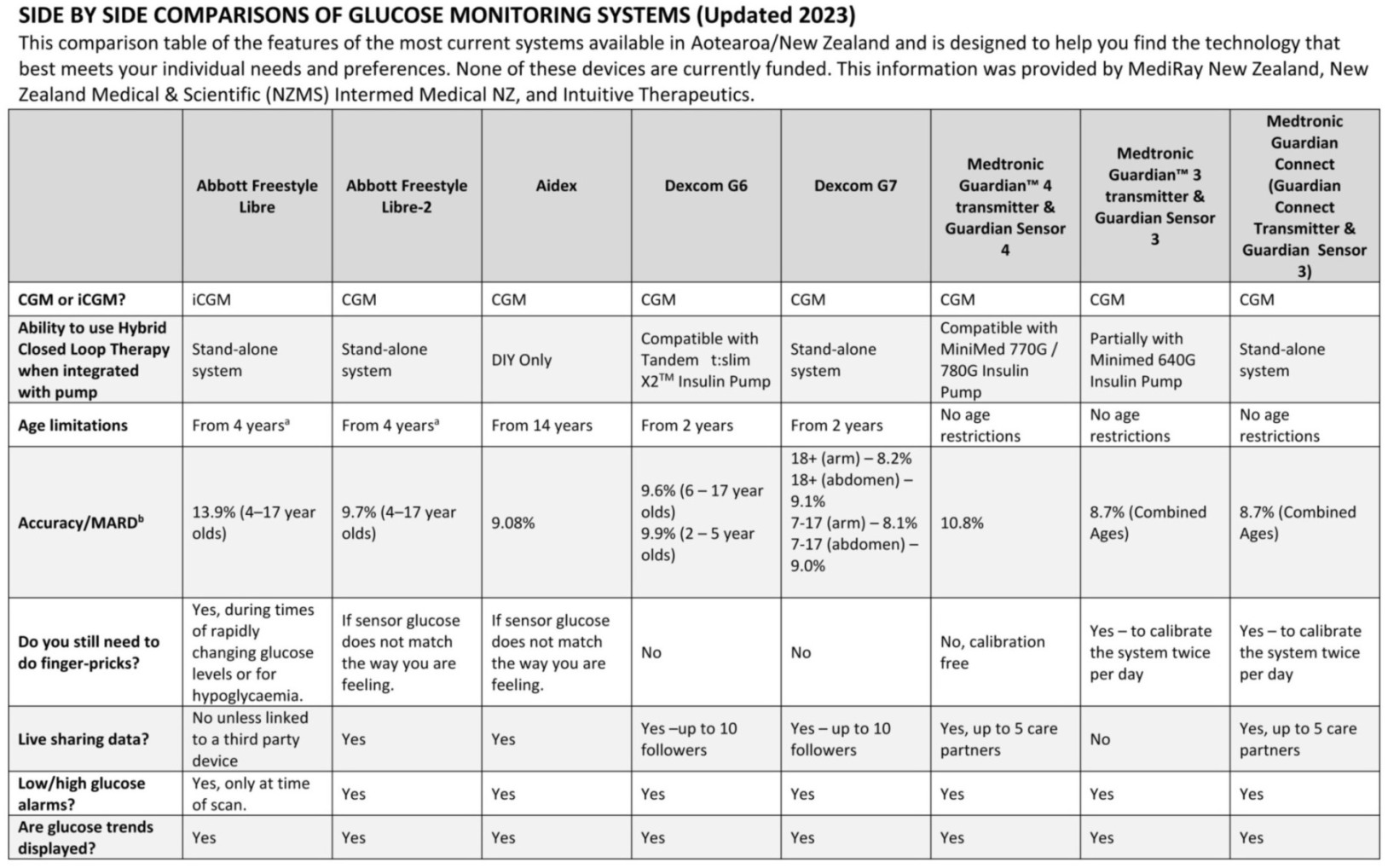
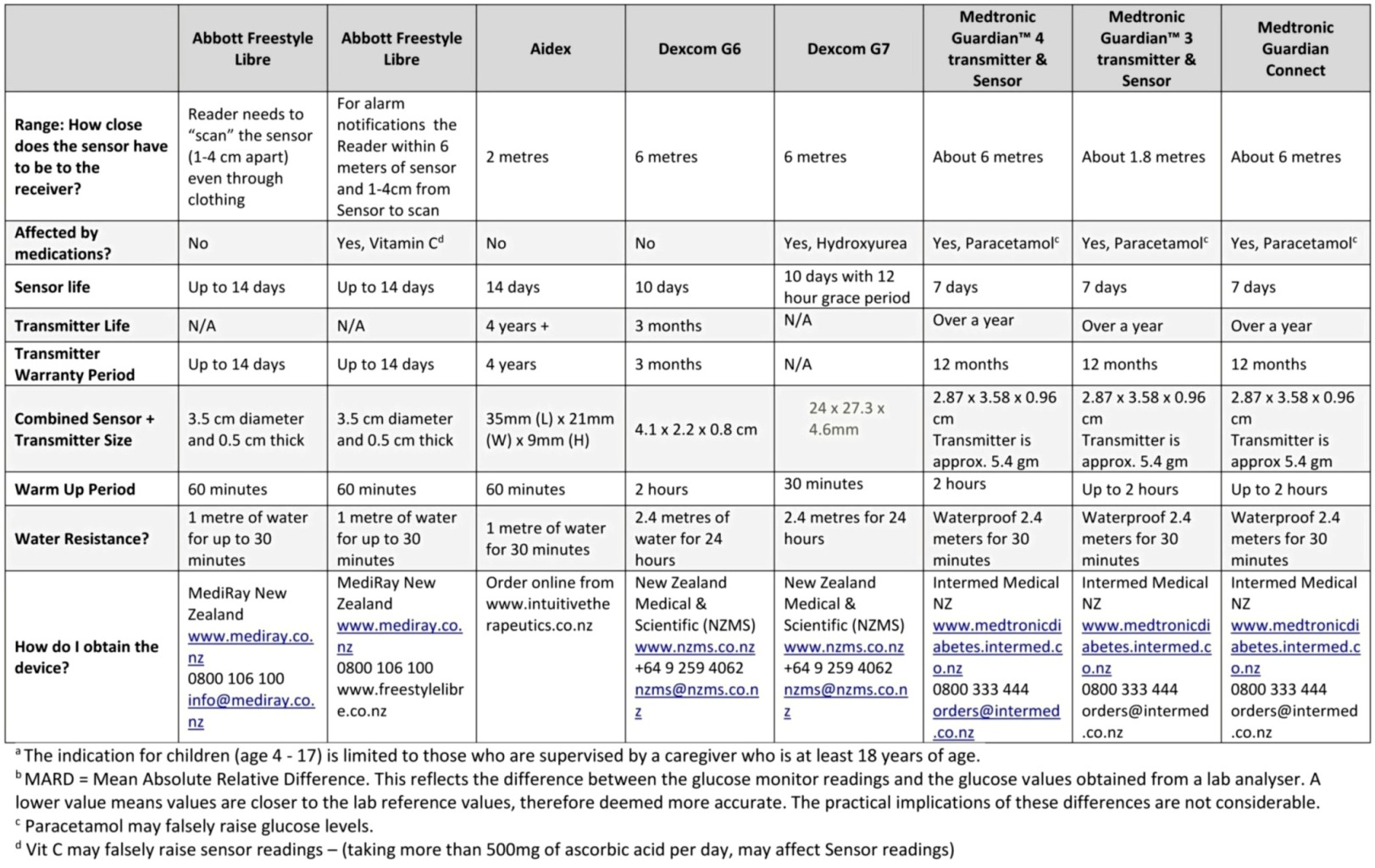
Side by side comparisons of Glucose Monitoring Systems
This comparison table of the features of the most current systems available (or going to be released) in New Zealand and is designed to help you find the technology that best meets your individual needs and preferences.
View or download the comparison table shown below via this link
Components of Continuous Glucose Monitoring Systems
The Sensor
A sensor is a thin, flexible wire (electrode, or filament) that sits just under the skin. It is inserted using an automatic insertion device, including an introducer needle (which is removed after insertion, leaving the sensor behind). The sensor is then held in place by an adhesive patch, in much the same way that an insulin pump infusion set is held to the skin. Once in place, the sensor is the part of the system that measures (“senses”) glucose levels, taking a glucose reading every 5 minutes. Sensors are disposable, when they reach the end of their approved life span they are removed and thrown out.
The Transmitter
The transmitter clips into the sensor housing; it takes the glucose reading obtained by the sensor and sends it out (via wireless signal) to a separate receiver. Transmitter batteries may be rechargeable and others are non-rechargeable and need to be replaced. Different manufacturers and models have different transmitter warranty periods.
The Receiver
The receiver “receives” the data from the transmitter and displays it in on different user interfaces. The receiver could be:
A stand-alone hand-held device or
An electronic device (smartphone or tablet) that contains the relevant software
Integrated into the display of the current pumps
For the data to be transmitted in real-time the receiver must stay within range of the transmitter.
Receiver Batteries
The battery-type for receivers depends on the model and vary from a replaceable (non-rechargeable) AA Lithium battery, to a custom rechargeable (not replaceable) battery. Non-replaceable batteries may need to be recharged every 3-5 days; the battery can be recharged for about a year and then the entire receiver may need to be replaced.
Glucose Information and Trends
The receiver displays the following information:
The current glucose reading
Past readings, displayed as a line graph, or glucose “trace” (24-hours on screen, and all past data via computer download)
Glucose trends: using arrows to show if your glucose is stable, rising or falling, AND how quickly glucose is changing
Glucose Alerts
A Continuous Glucose Monitoring Receiver can be set to give alerts:
High Glucose Alert tells you when your glucose level crosses an upper threshold that can be set by the user.
Low Glucose Alert tells you when your glucose level crosses a lower threshold that can be adjusted.
Rate of Change Alerts tell you is your glucose is rising or falling rapidly.
Out-of-Range Alert tells you when the receiver and transmitter are too far apart to communicate with each other.
“Replace Sensor” Notification tells you that the sensor life is almost up, and it is almost time to remove the current sensor.
Components of a Flash Glucose Monitoring System
The Sensor
A sensor is a thin flexible wire that sits just under the skin of the upper arm and is inserted using an automatic applicator. The sensor is then held in place by an adhesive patch, similar to an insulin pump infusion set. The sensor is the part of the system that actually measures (“senses”) glucose levels, taking a glucose reading every minute and storing those readings every 15 minutes. Sensors are disposable: they last for 14 days (at which point it automatically stops working). A new sensor then needs to be inserted to begin the next glucose monitoring cycle.
The Transmitter
The transmitter is integrated into the sensor pod (unlike a CGM transmitter, which is a separate component). It is therefore replaced when the sensor is replaced.
The Reader
The reader “reads” the data from the transmitter and displays the data on-screen. To access the glucose information, you simply “scan” the sensor by placing the reader within 1 cm to 4 cm of the sensor. The reader can access data readings though clothing (up to 4mm thick).
Flash glucose monitoring is not transmitted in real time and only shows data when the user “scans” the sensor with the reader. It is therefore important to scan sensors every 8 hours to avoid loss of data and current trends.
In order to talk to each other, the Libre reader needs to be held close to the transmitter. This system uses Near Field Communication (NFC), a secure and highly robust method of transmitting data between two devices, the same technology used by debit or credit card “tap” machines.
Reader batteries
The reader requires a rechargeable battery which lasts approximately 1 week.
Glucose information and trends
The reader stores up to 90 days of glucose readings (as long as you replace the sensor every 14 days and scan every 8 hours). The reader will also display:
The current glucose reading when scanned
Last 8 hours of data
Trend arrow indicating if glucose level is stable, rising, or falling and how quickly the glucose is changing.
How many days left in the sensor
Statistical data including average sensor glucose values and scanning frequency.
Glucose alerts
The FGM system does not have alerts for high or low glucose levels.
Advantages and limitations of Glucose Monitoring Systems
Advantages of All Glucose Monitoring Systems (CGM and FGM)
Reduced number of finger pricks - Glucose monitoring systems have the ability to measure glucose levels all the time and therefore finger pricks are not required as frequently as when using a blood glucose meter alone.
Ability to see patterns and trends - Glucose monitoring systems allow you to see where glucose levels have been and also where they are headed (arrows indicate glucose going ↑, ↓ or →). This means you can make informed decisions rather than educated guesses about the current glucose level. Glucose monitoring systems also provide a visual representation, in the form of line graphs, which can help you see pattern rather than just looking at “numbers”. This helps with determining the effectiveness of current basal and bolus insulin doses.
Accuracy – Although Blood Glucose Meters and Glucose Monitoring Systems measure different things (sensors measure glucose in interstitial fluid not blood), they have all been demonstrated through research to be accurate. This was done by comparing Glucose Monitoring Systems to well-established glucose analysers. MedSafe have also approved their use in New Zealand, providing further support for their accuracy.
Size of the device/s - The CGM and FGM sensors are both small in size and the Receiver/Reader differ depending on the device, but are usually close in size to a blood glucose monitor.
Data Management Systems - Data from both the CGM and FGM systems can be transferred to data management systems which can be accessed and shared with your health professionals who can help you analyse the data and discuss management options.
Limitations of all Glucose Monitoring Systems (CGM and FGM)
Financial cost – There is currently no funding for Glucose Monitoring Systems in New Zealand, so they come at a cost to the family. Costs differ depending on the device being purchased. Applicable costs can be found at the relevant company websites.
Data, data, data – Glucose monitoring systems produce a lot of data. It can be quite overwhelming to see all of the numbers, especially if you are new to managing diabetes. It is important to take the big picture approach and look at trends and patterns rather than focus on every individual number.
Burden of technology – Glucose monitoring systems are an additional device and for some people that is one device too many that reminds them about his/her diabetes. Alongside this is the additional learning to get the best out of the glucose monitoring system.
Skin reactions – Skin reactions (usually to the adhesive for the sensor), including rashes and irritation are possible at sensor sites. Some people are more sensitive than others to the adhesive of the systems. Cleanliness is also really important when changing sensors to reduce the risk of skin reactions and infections.
Pain or discomfort – Applying a sensor requires inserting a cannula into the skin. This can mean some discomfort. This is very much an individual experience and can be influenced by the site used, age of the user, and previous experiences.
Finger pricks are still needed – All the systems currently available in New Zealand will still require some finger pricks, although this is a lot less than if on finger pricks alone. Finger pricks are used alongside glucose monitoring systems for either calibration, prior to treatment of a low or correcting high blood glucose levels, or when glucose levels are changing quickly. This is because the interstitial fluid does not necessarily reflect the blood glucose level at that exact time. It is also important to use a finger prick when the number of the reader or receiver does not match any physical symptoms.
No system is fail-proof – No piece of technology is fail-proof. Always check glucose levels with a finger-prick blood glucose test if the child or young person has signs and symptoms of low or high blood glucose levels, even if FGM/CGM reading indicates a glucose level in target range.
Benefits Specific to Continuous Glucose Monitoring (CGM) Systems
Alerts – Continuous Glucose Monitoring Systems have the ability to set alarms for highs or lows. Both the Dexcom and Medtronic Systems also have alerts for when glucose levels are changing rapidly; which can help prevent hypoglycaemia or hyperglycaemia.
Observable from multiple devices – Continuous Glucose Monitoring Systems send data to a receiver, which may include an insulin pump and may also send data to additional devices including smartphones; allowing multiple observers of trends and glucose levels.
Improvement in glucose control – When used consistently CGM can reduce glucose variability, improve HbA1c, and reduce mild to moderate hypoglycaemia. This is an area of continued research in the paediatric population.
Integration with Insulin Pumps – Continuous Glucose Monitoring Systems can be integrated with specific pumps, meaning that no additional receiver is required. This is constantly advancing technology and the way CGM and insulin pumps interact.
Limitations Specific to Continuous Glucose Monitoring (CGM) Systems
Alerts – Some people find the alerts frustrating due to false readings. They can also lead to “alert fatigue”, where people start to ignore them. Alerts at night may also lead to sleep disruption.
Higher price point – CGM currently costs more than the FGM system.
Benefits Specific to Flash Glucose Monitoring (FGM) Systems
Longer sensor life – Sensors for the FGM System usually last 14 days.
Lower price point – The FGM System is cheaper than traditional CGM Systems.
Limitations Specific to Flash Glucose Monitoring (FGM) Systems
No alerts – There are no alerts on a FGM System, therefore unless you “scan” the sensor there is no indication of the current glucose level.
Only one reader – A single sensor can only pair with one reader. Therefore data cannot be transmitted to other people or “followers”.
Acknowledgements
The New Zealand Child and Youth Clinical Network (Paediatric Society of New Zealand) acknowledges the following organisations for allowing us to refer to their on-line resources in the development of this resource. For more information, tips and ideas from other families we encourage you to refer to these sites:
Waltzing the Dragon https://www.waltzingthedragon.ca/
Beyond Type 1 https://beyondtype1.org/
Disclaimer: The New Zealand Clinical Network for Children and Young People with Diabetes does not advocate for a specific manufacturer or supplier of glucose monitoring devices and do not have any funding from these companies.
